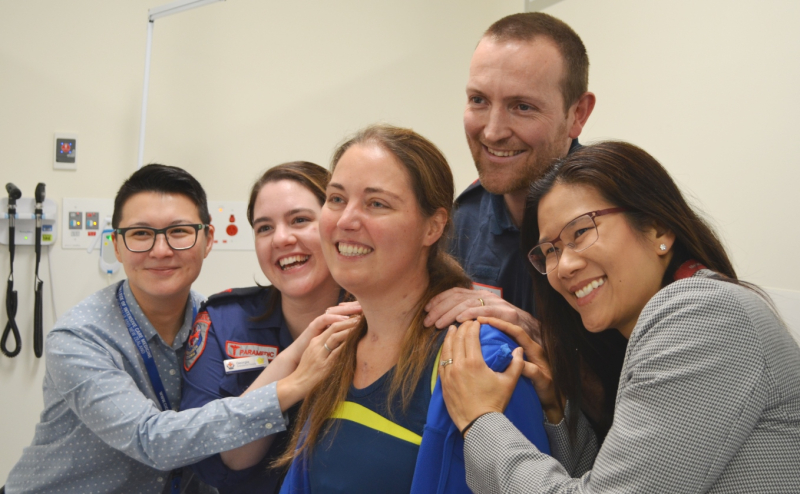
Heart attack, life support, transplant – Petra beats all odds
When Petra Brosch’s heart stopped beating during a routine run on Elwood beach, it was the beginning of a journey that would see The Alfred’s specialists drawing on the latest in cutting-edge medicine to save her life. The 35-year-old was suffering irreparable heart failure that would see her rely on life support, then an artificial heart and ultimately organ transplant.
Intensivist Dr Li Tan was part of the team who, in a high pressure and time critical environment, had to make the early decisions that would mean life or death.
Dr Tan was ready when a team of Ambulance Victoria paramedics brought Petra into the The Alfred’s Emergency and Trauma Centre in early May.
“She did not have a pulse, she did not have blood pressure and she was unconscious – she was in cardiac arrest,” Dr Tan said.
“At the time we had no idea why her heart had failed but, when she arrived in the emergency department, it took only a few minutes to decide that to give her the best chance of survival. We would need to put her on ECMO (extracorporeal membrane oxygenation)”, Dr Tan said.
Advanced life support using ECMO
Petra was given a special type of resuscitation called ECPR, or extracorporeal cardiopulmonary resuscitation, using ECMO.
“The only way that this was going to be successful is team work between the intensive care unit staff and the emergency department staff,” Dr Tan said.
During ECMO, a thin tube called cannula is inserted into the patient to remove blood, which is passed through a machine that gives it oxygen. The oxygenated blood is then returned to the patient through another cannula.
“ECMO provides support to vital organs, and in Petra’s case we were concerned about her brain, which is very vulnerable to damage without oxygen.”
Petra spent the next 12 hours under the care of ICU and heart specialists, who performed numerous medical interventions to help her live through the night. She suffered from internal bleeding and fluid in her lungs, which a cardiothoracic surgeon was able to relieve through surgery.
“It was an intense night, and I spent the rest of my shift by her bedside hoping she wouldn’t get worse,” Dr Tan said.
Petra spent the next two months in ICU
Dr Peter Bergin, Medical Director of the Heart Failure and Transplant Service at The Alfred, said there were no warning signs that Petra was born with an unusual heart. One of her arteries was positioned incorrectly, which eventually blocked the flow of blood and triggered a heart attack.
“We do not know why, on that particular evening on the beach, her heart failed,” said Dr Bergin, who added that this case was one of the most remarkable his team has seen.
Petra’s heart was severely damaged and could no longer work on its own. Prof David McGiffin, Head of Cardiothoracic Surgery at The Alfred, performed a unique and specialised procedure – he connected Petra’s heart to a mechanical pump on the outside of her chest.
Traditionally, the pump or LVAD (left ventricular assist device), is inserted into the patient’s chest. In Australia, it’s used in patients who are waiting for a heart transplant, and it can remain inside the body for years.
Petra was too unwell for the traditional LVAD, and her clinical team was concerned it may lead to blood clotting. However, it was critical to her survival that she receive the mechanical help so that she could stand up.
“In every operation where you’re in bed for a long period of time it means you are losing muscle. Petra’s muscles were wasting away – including vital muscles used for breathing – so we wanted to get her standing,” said Dr Bergin.
Petra, to the surprise of staff, stood up in ICU – an encouraging sign and a big step towards being eligible to go onto the heart transplantation list.
After two months in ICU, a heart became available
“It’s fair to say that because of our heritage of handling very sick patients, mechanical heart support and transplant, we are prepared to go in for the long-haul for all of our patients,” said Dr Bergin. “Because of our expertise and experience we are positioned and prepared to perform certain procedures that perhaps others wouldn’t – I don’t believe she would’ve survived if she hadn’t been brought to The Alfred.”
Petra is expected to get back to running and work, but she has a long road ahead.
“Her job now is to get strong, and we will help her,” said Dr Bergin. “The single most important person in this is Petra. Even with the fear of all of this, she’s happy, she’s smiling, loves life and she will continue to do well - she is an extraordinary young woman.”

_500_333.jpg)
