Aimee and Jamie

Imagine having the ability to change someone’s life with a phone call.
Aimee and Jamie, our transplant coordinators are the two people at The Alfred whose job it is to make the telephone call when a potentially life-saving organ becomes available for one of our patients. They see their patient’s lives transformed by the generosity of our organ donors.
The role of a transplant coordinator
Jamie: We work broadly across the heart and lung transplant service at The Alfred.
There are two major aspects to our role.
The first part is meeting and being involved in the care for potential transplant recipients, where we go through the stages of establishing their suitability to be a transplant recipient.
The most incredible part of the job is receiving calls from the donation agency, DonateLife. This phone call usually results in one of our patients receiving their life saving transplant.
When an organ is found for one of our patients
Amy: As soon as we receive the call from the donation agency, DonateLife, it’s go-go-go.
We begin by looking at the suitability of the organs for transplantation, working collaboratively with the different teams involved and then we set up for a transplant operation.
Making that call to the waiting list patient
Jamie: By the time we make that phone call, we have gotten to know the patient really well through their outpatient appointments.
Amy: Reactions can be quite varied but the most common reaction when we phone a person and tell them that we think we might have them a new heart or lungs, is one of ‘shock’. All rational thought goes out of the person’s head and sometimes panic sets in.
Some people are very practical and just get up and get straight to The Alfred, while others become quite emotional. They may scream with excitement or cry and many people get very short of breath.
Jamie: Sometimes patients need a bit of time to process the news – so we give them ten minutes and then call them back.
Often this call comes at 2 or 3am, so people will take longer to digest the information but we have to get straight down to business from the moment we make that telephone call.
Getting the patient to The Alfred
Jamie: Every minute counts. We have to give the patient instructions about preparing for the operation straight away- nothing else to eat or drink and a shower to start the skin preparation.
Some of these patients might live around the corner, so they can walk or drive in to The Alfred. Others might live in Queensland, Tasmania or South Australia, so that will involve us organising an urgent air ambulance to bring them to us at any time of the day or night.
The entire process is time critical; a patient receives the call and must leave their house in 30 minutes. The reality often strikes home for some patients at that point- they will not return to their home for three months, and that is if everything goes well.
Who’s going to deal with the dog? The cat? The kids? An entire life is suddenly put on hold.
Transporting the organs to the Alfred
Aimee: It is our responsibility to get the organ to theatre from wherever in Australia or New Zealand it may have come from. The furthest an organ will travel to us is from Western Australia (2,720km Perth-Melbourne) or New Zealand (2,405km from Christchurch - Melbourne).
Organs are transported in an esky on a charter flight if they’re arriving from a Perth, New Zealand or Darwin. Generally a team from our hospital will fly over, do the donor retrieval and travel back with the organ.
Every minute can be significant and part of our role is to manage the logistics around the organ retrieval so that the organ gets to the recipient as quickly as possible.
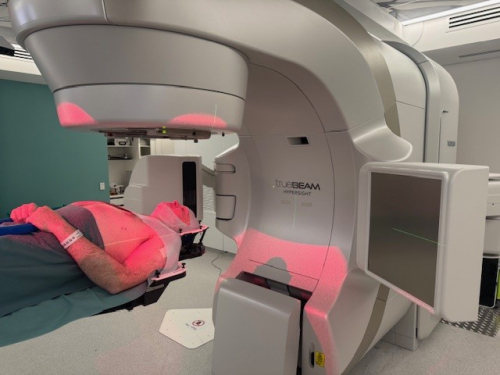
The surgery
Jamie: We are the first point of contact for the recipient when they arrive at the hospital- they come in through the Emergency Department and it is our role to meet them and check that they are ok and to talk them through the transplant.
Aimee: We go into theatre with the recipient and we coordinate the delivery of the organ to theatre. We stay in the operating room with the patient up until the organ arrives.
After the surgery
Aimee: Seeing someone get back to their life is undoubtedly the most rewarding part of my job.
It is amazing to see someone six months down the track, talking to you about their work or planning a holiday.
Jamie: It’s the fact that they can make plans again – 12 months before there was no capacity for survival and then we see them and they are going back to work and doing things that make their life meaningful.
Aimee: One of the problems I have and it is definitely a good problem, is that I often don’t recognise my old patients post-transplant because they look so well. I’ll often walk straight past them- we’ve only known them in their sick phase and six months post-transplant, they look like new people.
If you haven not registered your organ donor wishes
Jamie: Please, have the conversation. If you are unfortunate enough to be in a situation where you have to make the decision about whether a loved one should donate their organs, it helps so much to know their wishes.
Aimee: Overwhelmingly the reason people decline is because they didn’t know what their loved ones donation wishes were.
If someone’s donation wishes are known, consent rate from family jumps to 90 per cent.
We can tell you first-hand what a priceless gift organ donation is.
Register your donation wishes at Donate Life.